Molar Pregnancy: Symptoms, Causes, Diagnosis, and Treatment Explained
Pregnancy is usually a time of hope and excitement. However, in rare cases, abnormal tissue can develop inside the uterus instead of a healthy embryo — this condition is known as a molar pregnancy. Though it can be emotionally challenging, early diagnosis and proper medical treatment usually lead to a full recovery and the possibility of future healthy pregnancies.
This article explains everything you need to know about molar pregnancy, including its symptoms, causes, treatment options, and recovery process, supported by medical data from trusted sources such as the Mayo Clinic and the Cleveland Clinic.
Key Takeaways
- A molar pregnancy occurs when abnormal tissue grows in the uterus instead of a normal embryo.
- There are two main types: complete and partial molar pregnancy.
- Common symptoms include abnormal vaginal bleeding, unusually high hCG levels, and absence of a fetal heartbeat.
- Diagnosis is confirmed through ultrasound and blood tests.
- Treatment usually involves uterine evacuation (D&C) and careful follow-up to monitor hCG levels.
- Most women go on to have healthy pregnancies after treatment.
What Is a Molar Pregnancy?
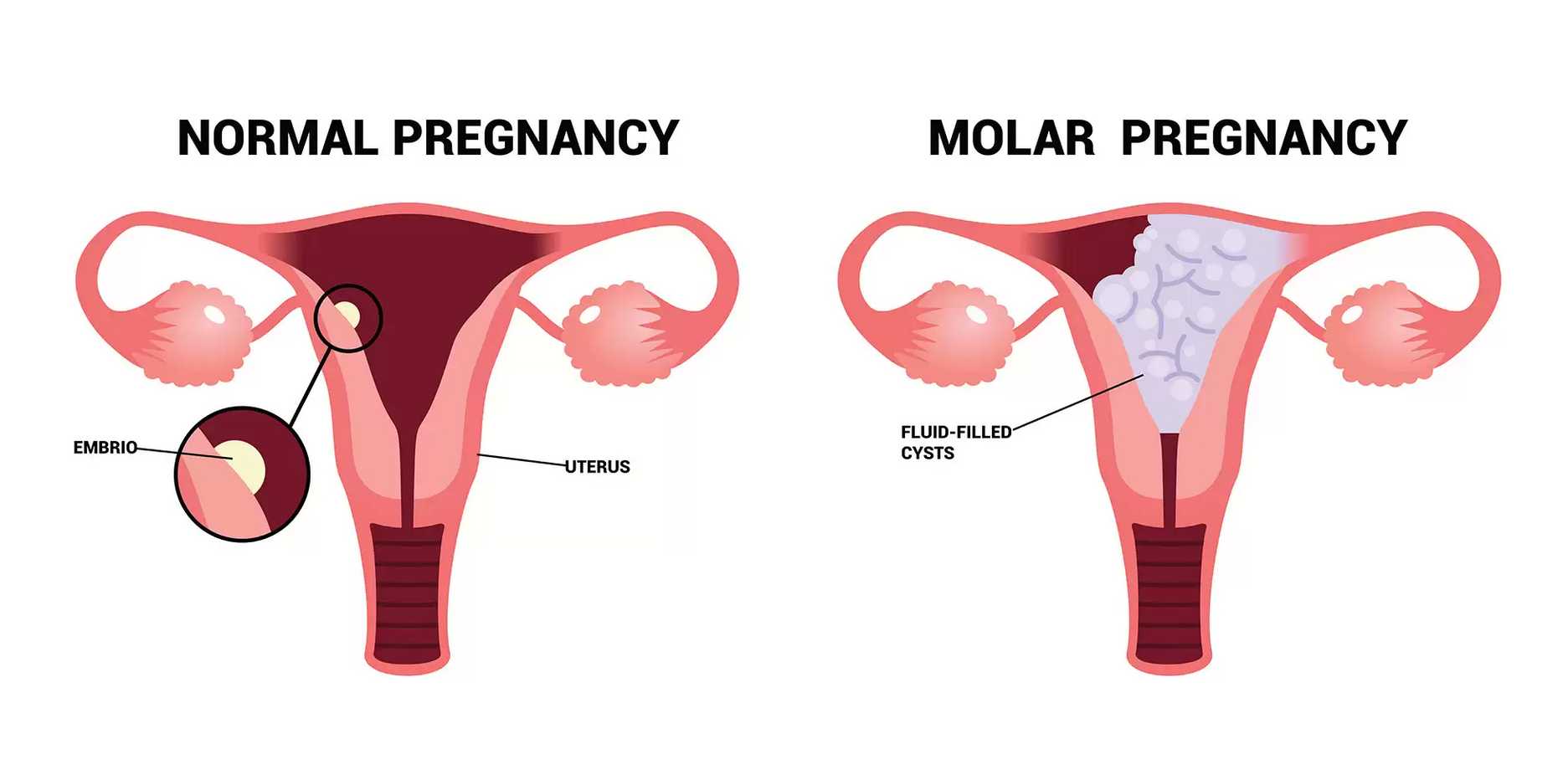
A molar pregnancy, also called a hydatidiform mole, is a rare complication of pregnancy caused by abnormal fertilization. Instead of forming a normal embryo and placenta, the fertilized egg develops into a cluster of fluid-filled cysts.
This condition belongs to a group of disorders known as gestational trophoblastic diseases (GTDs), which involve the abnormal growth of placental tissue.
| Normal Pregnancy | Molar Pregnancy |
|---|---|
| Embryo develops normally | No viable embryo |
| Placenta nourishes the fetus | Abnormal tissue forms cysts |
| Normal hCG levels | Extremely high hCG levels |
Types of Molar Pregnancy
Complete Molar Pregnancy
In a complete molar pregnancy, there is no embryo or normal placental tissue. The uterus fills entirely with abnormal cells. This usually happens when an empty egg is fertilized by one or two sperm, leading to duplicated paternal chromosomes.
Partial Molar Pregnancy
A partial molar pregnancy occurs when an abnormal embryo forms along with some normal placental tissue. However, it cannot develop into a viable baby because it has too many chromosomes — typically 69 instead of 46.
What Causes a Molar Pregnancy?
A molar pregnancy results from genetic errors during fertilization. These errors cause abnormal cell growth and the development of cyst-like tissue instead of a fetus.
Common Risk Factors
- Maternal age under 20 or over 40
- Previous molar pregnancy
- Nutritional deficiencies (especially low vitamin A or carotene)
- A history of miscarriage or fertility treatments
Molar pregnancy affects roughly 1 in every 1,000 pregnancies, though rates are slightly higher in some parts of Asia and Latin America.
Symptoms of a Molar Pregnancy
The symptoms often resemble those of a normal pregnancy at first, but certain warning signs can help distinguish a molar pregnancy:
- Vaginal bleeding, usually dark brown or bright red
- Rapid uterine growth (larger than expected for gestational age)
- Severe nausea or vomiting (hyperemesis gravidarum)
- High hCG levels without detection of a heartbeat
- Pelvic pressure or pain
- Preeclampsia symptoms before 20 weeks (unusual in normal pregnancies)
| Typical Pregnancy | Molar Pregnancy |
|---|---|
| Gradual uterine growth | Rapid enlargement |
| Mild morning sickness | Severe nausea and vomiting |
| Detectable fetal heartbeat | No heartbeat |
| Normal hCG levels | Extremely elevated hCG |
How Is a Molar Pregnancy Diagnosed?
Diagnosis typically involves a combination of imaging and laboratory tests:
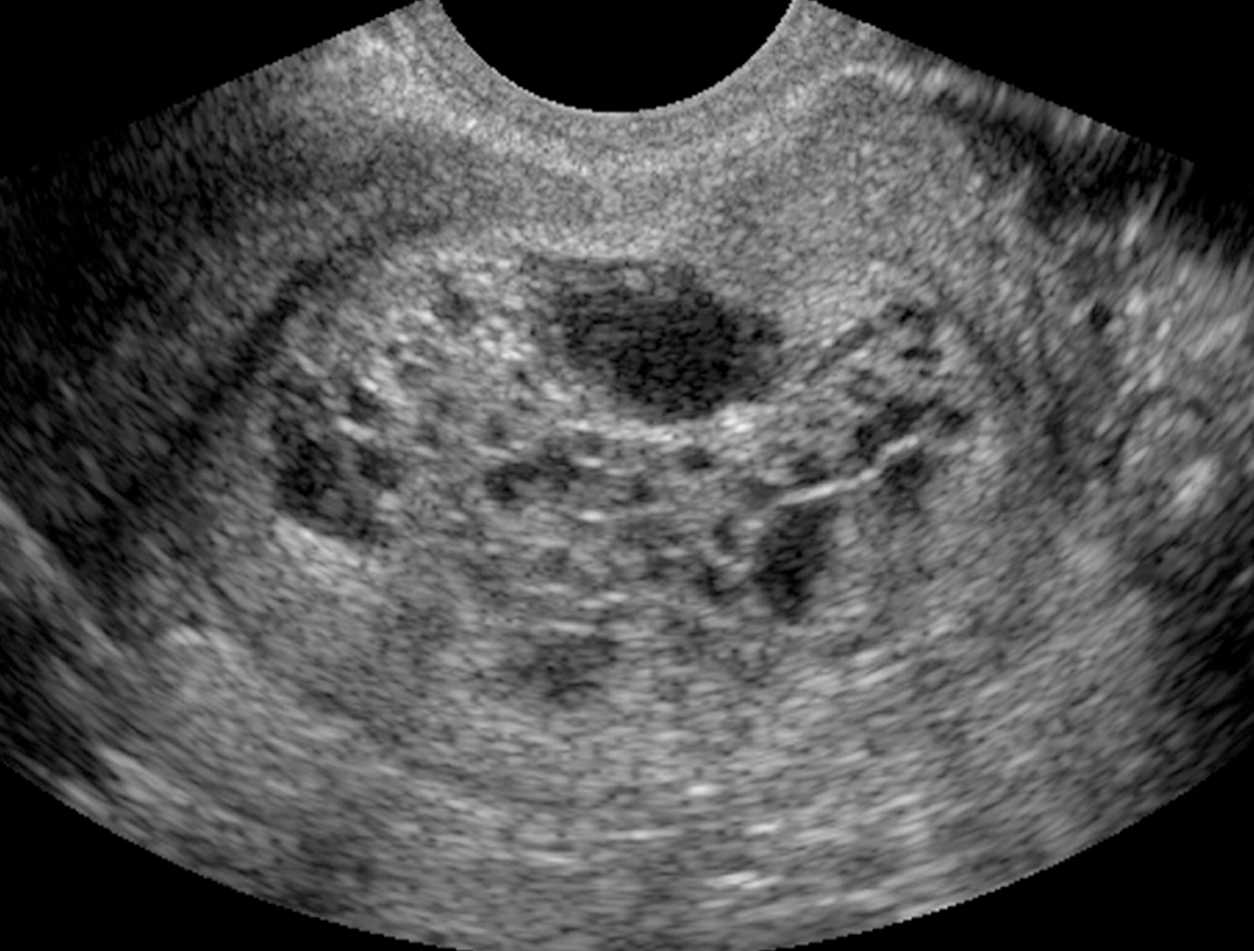
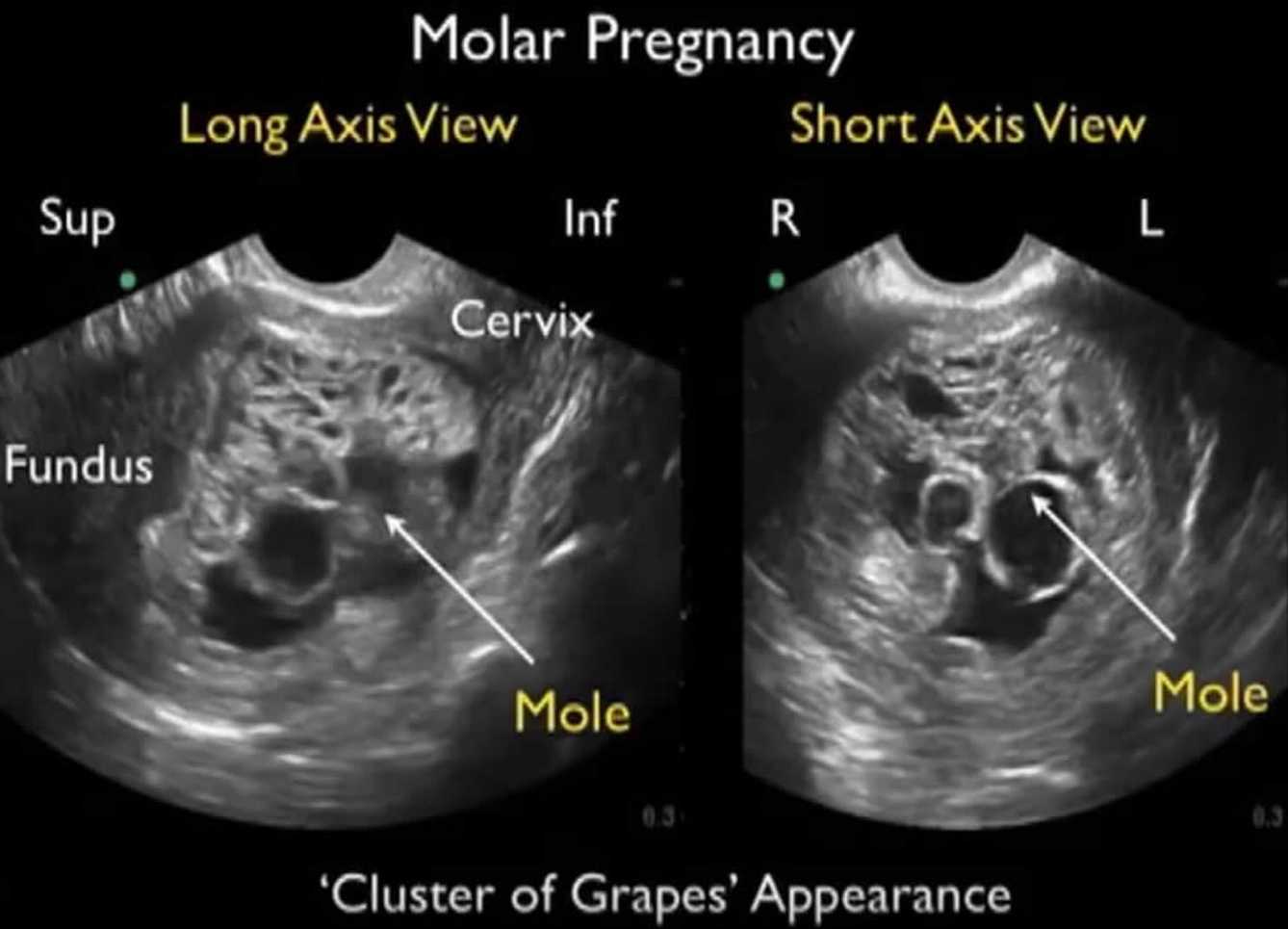
Ultrasound Examination
A transvaginal ultrasound often reveals a distinctive “snowstorm” or “cluster of grapes” appearance — abnormal tissue with no fetus or amniotic fluid.
Blood Tests
High levels of human chorionic gonadotropin (hCG) that exceed the expected range for gestational age often suggest a molar pregnancy.
Tissue Examination
After uterine evacuation, the tissue is analyzed under a microscope to confirm the diagnosis and rule out other gestational trophoblastic diseases.
Treatment for Molar Pregnancy
The main goal of treatment is to remove the abnormal tissue and prevent complications.
Uterine Evacuation (Dilation and Curettage – D&C)
A minor surgical procedure is performed under anesthesia to gently remove the molar tissue from the uterus.
Monitoring and Follow-Up
After treatment, hCG levels are monitored weekly or monthly until they return to normal. Persistent elevation may indicate remaining molar tissue.
- During this period, patients are advised not to become pregnant for at least 6–12 months.
- Effective contraception is recommended to avoid confusion in test results.
Chemotherapy (in Rare Cases)
If hCG levels remain high or if molar cells spread to other areas, mild chemotherapy (often methotrexate) may be required. This is rare and highly treatable.
| Treatment Step | Purpose | Timeline |
|---|---|---|
| D&C procedure | Remove molar tissue | Immediate |
| hCG monitoring | Detect recurrence | 6–12 months |
| Contraceptive use | Prevent new pregnancy | During follow-up |
| Chemotherapy (if needed) | Treat persistent GTD | Case-dependent |
Can You Get Pregnant Again After a Molar Pregnancy?
Yes — most women who experience a molar pregnancy later go on to have healthy, normal pregnancies. Once hCG levels have returned to zero and the follow-up period has ended, fertility typically returns to normal.
Doctors usually recommend waiting 6 to 12 months before trying to conceive again. Emotional recovery is also important, and counseling or support groups can be beneficial.
🌼 Support Resources:
How to Reduce the Risk of Molar Pregnancy
While not all cases can be prevented, you can reduce risk factors by following these molar pregnancy prevention guidelines:
- Maintain a balanced diet rich in vitamin A and folate.
- Attend all prenatal check-ups and report unusual symptoms early.
- If you’ve had a molar pregnancy before, request early ultrasound monitoring in future pregnancies.
Frequently Asked Questions About Molar Pregnancy
Can a molar pregnancy turn cancerous?
In rare cases, persistent molar tissue can develop into choriocarcinoma, a fast-growing but highly treatable cancer.
Is molar pregnancy hereditary?
No, it usually occurs due to random genetic errors during fertilization.
How long does it take for hCG levels to normalize?
Typically within 8–12 weeks after uterine evacuation.
Can I detect a molar pregnancy with a home test?
Home pregnancy tests cannot distinguish between normal and molar pregnancies — only medical imaging and lab tests can confirm it.
Conclusion
A molar pregnancy can be a frightening and emotional experience, but with prompt diagnosis and treatment, the prognosis is excellent. Most women make a full recovery and can later have healthy pregnancies.
If you experience unusual bleeding, excessive nausea, or rapid uterine growth during pregnancy, contact your healthcare provider right away. Early intervention is the best way to protect your health and future fertility.
Stay informed and proactive — follow your doctor’s recommendations, monitor your recovery, and connect with support networks. Knowledge is your strongest ally in regaining confidence and hope after a molar pregnancy.